Fertility Treatment Options
Ovulation Induction (OI) / Controlled Ovarian Hyperstimulation (COH)

Ovulation induction is a fertility treatment that stimulates the growth of an egg and subsequent ovulation, thereby allowing pregnancy to occur.
Controlled ovarian hyperstimulation (a.k.a. ovarian hyperstimulation or superovulation) is a fertility treatment that stimulates the growth and subsequent ovulation of multiple eggs, thereby increasing the likelihood of pregnancy.
Reasons for Ovulation Induction / Controlled Ovarian Hyperstimulation:
- Lack of ovulation (absent or irregular menstruation)
- Infrequent or irregular ovulation (infrequent or irregular menstruation)
- Unable to determine when ovulation occurs
- Short luteal phase duration
- Unexplained infertility
Description:
Typically on the third day of menstruation, oral medication for 5 days or subcutaneous gonadotropin injections for 1-2 weeks stimulate the ovaries to grow one or more eggs. Ultrasounds and hormone blood tests will be performed to closely monitor ovarian follicle development. Intrauterine insemination (IUI) and/or sexual intercourse will be timed with ovulation to increase the likelihood of pregnancy. Progesterone supplementation is added to maximize the success of embryo implantation into the uterine wall.
Intrauterine Insemination (IUI)
Intrauterine insemination (a.k.a. artificial insemination or insemination) is a fertility treatment that places concentrated sperm directly inside a woman’s uterus to increase the number of motile sperm that reaches the ovulated egg(s), thereby increasing the likelihood of pregnancy.
Reasons for Intrauterine Insemination:
- Low sperm count
- Decreased sperm motility
- Sperm size or shape abnormalities
- Erectile or ejaculatory dysfunction
- Cervical abnormalities
- Antisperm antibodies
- Semen allergy
- Unexplained infertility
- Donor sperm
Description:
Semen is collected from the male partner or donor sperm is purchased. This sample is "washed" to remove unwanted seminal fluid elements, resulting in highly concentrated motile sperm. A soft catheter is used to carefully place the sperm directly into the uterine cavity on the day of ovulation. 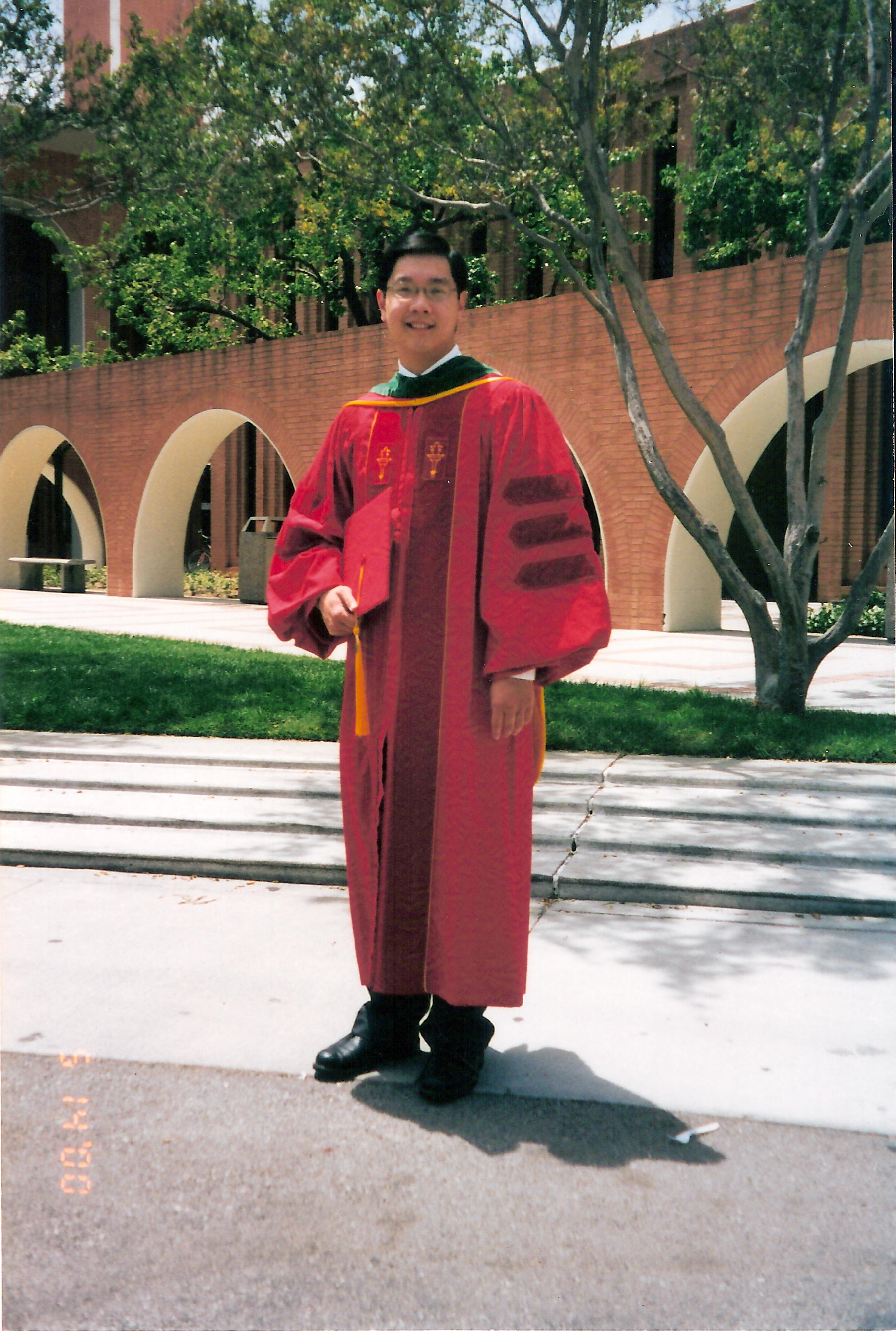 The increased number of motile sperm reaching the egg(s) increases the pregnancy rate. The intrauterine insemination is typically painless. After the intrauterine insemination, the woman will rest for a short period of time and then resume her normal activities.
The increased number of motile sperm reaching the egg(s) increases the pregnancy rate. The intrauterine insemination is typically painless. After the intrauterine insemination, the woman will rest for a short period of time and then resume her normal activities.
In Vitro Fertilization (IVF)
In vitro fertilization (a.k.a. test tube baby) is the most technologically advanced and most successful fertility treatment where multiple eggs are stimulated to grow, the eggs are fertilized by sperm outside of the body, and the resulting embryo(s) are transferred directly into the woman’s uterus to greatly increase the likelihood of pregnancy. The benefits of in vitro fertilization include: numerous eggs are collected, minimal sperm is required, fallopian tubes are bypassed, poor natural fertilization of the egg by sperm can be detected, embryo growth competency is observed, preimplantation genetic testing can be performed, sex selection for male or female child is possible, donor eggs can be used to achieve a pregnancy, and a gestational surrogate can be used to carry the pregnancy.
Reasons for In Vitro Fertilization:
- Fertilization abnormalities (sperm difficulty in penetrating the egg)
- Recurrent pregnancy loss
- Preimplantation genetic diagnosis (PGD)
- Preimplantation genetic screening (PGS)
- Ovulatory dysfunction
- Antisperm antibodies
- Unexplained infertility
- Fertility preservation – egg and embryo freezing
- Donor eggs
- Gestational surrogate
- Sex (gender) selection

Description:
Pretreatment with 1-3 weeks of birth control pills for ovarian suppression generally yields a greater number of mature eggs. After pretreatment, subcutaneous gonadotropin injections for 1-2 weeks stimulate the ovaries to grow multiple eggs. Ultrasounds and hormone blood tests will be performed to closely monitor ovarian follicle development. Under anesthesia, these eggs are retrieved by an ultrasound-guided needle through the vaginal wall as an outpatient procedure. The eggs are separated and fertilized that same day by either placing sperm on top of each egg for natural fertilization or injecting one sperm directly into each egg, which is called intracytoplasmic sperm injection (ICSI). The resulting embryos are grown for 3-5 days. Assisted hatching (AH) may be performed to make a small hole in the outer shell of the embryo to aid implantation. The embryos can be biopsied for preimplantation genetic diagnosis (PGD) or screening (PGS) to detect single gene disorders, structural and numerical chromosomal errors such as Down’s syndrome, and the sex (gender) of each embryo. Selected embryo(s) is/are then delicately transferred into the uterus using a soft catheter under ultrasound guidance. The woman typically rests for 48 hours after embryo transfer. Estrogen and progesterone supplementation are added to maximize the success of embryo implantation into the uterine wall. Excess embryos are generally frozen by the vitrification technique and stored for later use.
Fertility Preservation – Egg Freezing
Egg freezing (a.k.a. oocyte cryopreservation) for fertility preservation is the newest technological breakthrough that allows women to stop their reproductive biological clock by freezing and storing eggs until pregnancy is desired. Egg freezing is a great option for women delaying childbearing due to educational studies, career advancement, achieving personal goals, or still awaiting the right life partner.
For women diagnosed with cancer, treatment with surgery, chemotherapy and/or radiation can destroy the eggs in their ovaries leading to subfertility with difficulty conceiving a child or sterility without the ability to conceive a child with one’s own genetic material. Fertility preservation by egg or embryo freezing is strongly recommended as the best opportunity for children with one’s own genetic material in the future.
Description:
 Pretreatment with 1-3 weeks of birth control pills for ovarian suppression generally yields a greater number of mature eggs. With cancer patients, this pretreatment is skipped to minimize the delay before cancer treatment. Subcutaneous gonadotropin injections for 1-2 weeks stimulate the ovaries to grow multiple eggs. Ultrasounds and hormone blood tests will be performed to closely monitor ovarian follicle development. Under anesthesia, these eggs are retrieved by an ultrasound-guided needle through the vaginal wall as an outpatient procedure. All mature eggs are immediately frozen by the vitrification technique. In vitro maturation (IVM) will be performed overnight on the immature eggs and additional mature eggs may be frozen the day after retrieval.
Pretreatment with 1-3 weeks of birth control pills for ovarian suppression generally yields a greater number of mature eggs. With cancer patients, this pretreatment is skipped to minimize the delay before cancer treatment. Subcutaneous gonadotropin injections for 1-2 weeks stimulate the ovaries to grow multiple eggs. Ultrasounds and hormone blood tests will be performed to closely monitor ovarian follicle development. Under anesthesia, these eggs are retrieved by an ultrasound-guided needle through the vaginal wall as an outpatient procedure. All mature eggs are immediately frozen by the vitrification technique. In vitro maturation (IVM) will be performed overnight on the immature eggs and additional mature eggs may be frozen the day after retrieval.
When pregnancy is desired, the eggs will be thawed and fertilized by intracytoplasmic sperm injection (ICSI). The resulting embryos will be grown for 3-5 days. Assisted hatching (AH) will be performed to make a small hole in the outer shell of the embryo to aid implantation. The embryos can be biopsied for preimplantation genetic diagnosis (PGD) or screening (PGS) to detect single gene disorders, structural and numerical chromosomal errors such as Down’s syndrome, and the sex (gender) of each embryo. The selected embryo(s) will then be delicately transferred into the uterus.
Fertility Preservation – Embryo Freezing
Embryo freezing (a.k.a. embryo cryopreservation) for fertility preservation allows women to stop their reproductive biological clock by freezing and storing embryos until pregnancy is desired. Embryo freezing is a great option for women delaying childbearing due to educational studies, career advancement, achieving personal goals, or scheduling the optimal time to expand the family.
For women diagnosed with cancer, treatment with surgery, chemotherapy and/or radiation can destroy the eggs in their ovaries leading to subfertility with difficulty conceiving a child or sterility without the ability to conceive a child with one’s own genetic material. Fertility preservation by egg or embryo freezing is strongly recommended as the best opportunity for children with one’s own genetic material in the future.
Description:
Pretreatment with 1-3 weeks of birth control pills for ovarian suppression generally yields a greater number of mature eggs. In cancer patients, this pretreatment is skipped to minimize the delay before cancer treatment. Subcutaneous gonadotropin injections for 1-2 weeks stimulate the ovaries to grow multiple eggs. Ultrasounds and hormone blood tests will be performed to closely monitor ovarian follicle development. Under anesthesia, these eggs are retrieved by an ultrasound-guided needle through the vaginal wall as an outpatient procedure. The eggs are separated and fertilized by either placing sperm on top of each egg or through intracytoplasmic sperm injection (ICSI). The resulting embryos are grown for 2-5 days and frozen by the vitrification technique. The embryos can be biopsied for preimplantation genetic diagnosis (PGD) or screening (PGS) to detect single gene disorders, structural and numerical chromosomal errors such as Down’s syndrome, and the sex (gender) of each embryo prior to freezing.
When pregnancy is desired, the embryo(s) will be thawed and assisted hatching (AH) performed to make a small hole in the outer shell of the embryo to aid implantation. The embryo(s) will then be delicately transferred into the uterus.
Egg Donor / Sperm Donor
IVF Fertility Center has comprehensive third party reproduction services, including egg donation and sperm donation. Egg donation and sperm donation can be through 2 sources: 1) known (a.k.a. directed) family member, relative or acquaintance, or 2) unknown (a.k.a. anonymous) through an agency or bank. We work closely with many well-established and reputable third party agencies and banks.
Intracytoplasmic Sperm Injection (ICSI)
Intracytoplasmic sperm injection is a technique used during in vitro fertilization (IVF) in which a single sperm is injected directly into a mature egg, thereby increasing the likelihood of fertilization.
Reasons for Intracytoplasmic Sperm Injection:

- Limited sperm available
- Sperm was surgically extracted from the testes
- Severe sperm abnormalities
- Fertilization abnormalities (sperm difficulty in penetrating the egg)
- Antisperm antibodies
- Limited eggs retrieved with IVF
- Frozen-thawed sperm used
- Frozen-thawed eggs used
- Preimplantation genetic diagnosis (PGD)
- Preimplantation genetic screening (PGS)
- Sex (gender) selection
- Unexplained infertility
Description:
Following egg retrieval from the woman’s ovaries during IVF treatment, the eggs are prepared by removing the surrounding cells. Under high-power magnification, the mature egg is held in place by gentle suction using a glass pipe tte. A singe sperm is selected, immobilized by removing its tail, and drawn into a microscopic glass needle. The microscopic needle penetrates the outer shell of the egg and the sperm is injected directly into the cytoplasm of the mature egg. The fertilized egg is placed into the incubator and monitored for embryo growth during the next 3-5 days. IVF is completed by delicately transferring selected embryo(s) into the uterus.
tte. A singe sperm is selected, immobilized by removing its tail, and drawn into a microscopic glass needle. The microscopic needle penetrates the outer shell of the egg and the sperm is injected directly into the cytoplasm of the mature egg. The fertilized egg is placed into the incubator and monitored for embryo growth during the next 3-5 days. IVF is completed by delicately transferring selected embryo(s) into the uterus.
Assisted Hatching (AH)
Assisted hatching is a technique used during in vitro fertilization (IVF) in which a small opening is made in the zona pellucida or outer protective shell of the embryo, thereby increasing the likelihood of embryo implantation into the uterine wall.
Reasons for Assisted Hatching:
- Embryos with thick zona pelucida
- Poor embryo quality
- Older women (advanced maternal age)
- Women with high basal FSH level
- Failed IVF treatments
- Frozen-thawed embryos used
- Frozen-thawed eggs used
- Preimplantation genetic diagnosis (PGD)
- Preimplantation genetic screening (PGS)
- Sex (gender) selection
Description:
Before embryo transfer into the uterus during IVF treatment, each suitable embryo is held in place by gentle suction using a glass pipette under high-power magnification. The zona pellicida or outer protective shell of the embryo is opened by microlaser, acidic solution, or mechanical micromanipulation. This opening allows the embryo to easily “hatch” out of its outer protective shell, which must occur before implantation into the uterine wall. IVF is completed by delicately transferring selected embryo(s) into the uterus.
Preimplantation Genetic Diagnosis (PGD)
Preimplantation genetic diagnosis is a technique used during in vitro fertilization (IVF) in which embryos are tested for any genetic disorder caused by identified gene mutation(s) or known numerical and structural chromosomal abnormalities. A couple with a known genetic abnormality can prevent their children from inheriting their genetic abnormality. Only embryos without the genetic abnormality will be transferred into the uterus.
Additionally, preimplantation genetic diagnosis can be used for sex (gender) selection and human leukocyte antigen (HLA) matching. When a child is affected by an illness requiring stem cell transplantation, such as leukemia or lymphoma, parents can test embryos for a HLA-compatible match in order to have another child that can donate stem cells to their ill brother or sister.
Description:
Following egg retrieval from the woman’s ovaries during IVF treatment, egg fertilization by intracytoplasmic sperm injection (ICSI) is recommended to improve the accuracy of PGD. The resulting embryo is allowed to grow normally in the incubator for 3 days. At this 8 cell embryo stage, assisted hatching (AH) is performed to make a small opening in the zona pellucida or outer protective shell of the embryo. A single cell from the embryo is gently removed for genetic testing. IVF is completed by delicately transferring embryo(s) without the genetic abnormality into the uterus.
Preimplantation Genetic Screening (PGS)
Preimplantation genetic screening is a technique used during in vitro fertilization (IVF) in which embryos can be tested for numerical and structural chromosomal abnormalities, such as Down syndrome (trisomy 21). All 46 human chromosomes (22 pairs of autosomes, X chromosome, and Y chromosome) are genetically screened. Sex (gender) selection is performed at the same time. The benefit of preimplantation genetic screening is to assure that only chromosomally normal embryos are transferred into the uterus.
Description:
Following egg retrieval from the woman’s ovaries during IVF treatment, egg fertilization by intracytoplasmic sperm injection (ICSI) is recommended to improve the accuracy of PGS. The resulting embryo is allowed to grow normally in the incubator for 5-6 days. At this blastocyst embryo stage (70-100 cells), assisted hatching (AH) is performed to make a small opening in the zona pellucida or outer protective shell of the embryo. Multiple cells from the trophectoderm (future placenta) are gently removed for genetic screening. The inner cell mass (future fetus) is not disturbed. IVF is completed by delicately transferring chromosomally normal embryo(s) into the uterus during the same IVF cycle, or chromosomally normal embryos are frozen and transferred into the uterus in a subsequent cycle.
Sex (Gender) Selection
During in vitro fertilization (IVF), each embryo can be tested for sex (gender) with virtually 100% accuracy using the technique of preimplantation genetic diagnosis (PGD) or preimplantation genetic screening (PGS). The benefit of preimplantation sex (gender) selection is to assure that only embryo(s) of the desired sex (gender) are transferred into the uterus for the purpose of family balancing.
Description:
Following egg retrieval from the woman’s ovaries during IVF treatment, egg fertilization by intracytoplasmic sperm injection (ICSI) is recommended to improve the accuracy of sex (gender) determination. The resulting embryo is allowed to grow normally in the incubator for 3 days with the PGD technique or 5-6 days with the PGS technique. Assisted hatching (AH) is performed to make a small opening in the zona pellucida or outer protective shell of the embryo. A single cell from the embryo is gently removed for genetic testing with PGD or multiple cells from the trophectoderm (future placenta) are gently removed for genetic screening with PGS. IVF is completed by delicately transferring embryo(s) of the desired sex (gender) into the uterus.
Reproductive Surgery
Dr. John Kuo has vast experience in the surgical treatment for fertility and reproduction. In his many years as a professor at the University of California, Los Angeles (UCLA), he has trained numerous Obstetrics and Gynecology residents and Reproductive Endocrinology and Infertility fellows. Surgical options for fertility include laparotomy, laparoscopy, and hysteroscopy.
Laparoscopy is a minimally invasive surgical technique for infertility diagnosis and treatment. A camera is inserted into the abdominal cavity through a small incision just under the navel. It allows direct visual examination of the uterus, fallopian tubes, ovaries, and pelvis. Laparoscopic surgery is used to open blocked fallopian tubes, remove ovarian cysts, remove scar tissue around the fallopian tubes and ovaries, treat endometriosis, and remove uterine fibroids.
Hysteroscopy is another minimally invasive surgical technique for infertility diagnosis and treatment. A camera is inserted into the uterine cavity through the cervix, without any incision. It allows direct visual examination of the uterine cavity. Hysteroscopic surgery is used to remove endometrial polys, remove uterine fibroids, treat an intrauterine septum, open blocked fallopian tubes, and remove scars within the uterine cavity.



